The human relationship with bacteria is an ancient and complex one. As the first life forms to colonise the earth around 3.8 billion years ago, bacteria (and other single-celled organisms) have had some time to evolve to suit their surroundings. Bacteria live everywhere – from hydrothermal vents at the bottom of the ocean to Arctic permafrost – but thrive particularly well within the human body. Similarly, we can’t live without them. We actually carry more bacterial cells than human ones, primarily in our gut and on the surface of our skin. Pathogenic bacteria – those that cause us harm – are diverse and prevalent across every continent, and cause a multitude of diseases.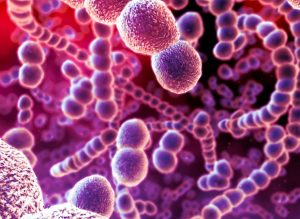
Developing a drug which fights pathogenic bacteria, whilst maintaining the body’s beneficial species, was a feat overcome by Alexander Fleming in 1928, with the development of penicillin. These days, it’s hard to imagine a world where simple infections such as tonsillitis cannot be treated with antibiotics, but scientists and clinicians are becoming increasingly wary of the resistance of bacteria to the most widely-used and relied upon drugs. Life science companies – including manufacturers of scientific instruments – are stepping up to develop novel solutions to this crisis, utilising increasingly sophisticated technology spanning fields such as proteomics, genomics and personalised medicine.
A brief history of antibiotics
Although the most recognised landmark in the history of antibiotic development was Fleming’s penicillin, the use of other microorganisms such as fungi to tackle bacterial infection goes back to early ancient history. For example, Greeks and Indians used moulds and other plants to treat infections, whilst ancient Egyptians used mouldy bread to treat infected wounds. Penicillin received the nickname “the wonder drug” as it saved the lives of countless throughout World War II – those who not only picked up infections in the field but in hospitals as well.
As well as on the frontline, the introduction of antibiotics into mainstream medicine meant that previously deadly infections, such as pneumonia and tuberculosis, could be readily treated. Life-saving surgery also became more viable, as the likelihood infected incisions becoming life-threatening was minimised.
How the drugs work
There are two general categories of antibacterial therapeutic treatment:
- Empiric therapy – when the specific bacterial species causing infection has not yet been identified, broad-spectrum antibiotics are administered, often pending lab test results to identify the causative bacteria.
- Targeted/definitive therapy – if the pathogenic bacteria is already known or has been categorised based on lab tests, antibiotics which target specific species of bacteria (narrow-spectrum) are used.
Where possible, hospitals and health trusts favour the use of targeted therapy, as it saves money, reduces toxicity and unnecessary side-effects, and slows down the emergence of antibiotic resistance.
Antibiotic resistance 101
Being named one of the greatest global threats of the 21st Century and frequently reported in mainstream news, antibiotic resistance is a well-known term across the world. But what does it really mean and why is it such a problem?
One species of bacteria can encompass multiple different strains: the genetic code of each strain differs very slightly and each tiny change (or mutation) in this code can confer resistance to the specific drug that has been designed to kill it. This selective resistance builds when someone is treated with antibiotics and the resistant strain survives, while the susceptible strains die. The resistant strains then multiply and, to make matters worse, antibacterial resistance genes can be exchanged between different bacterial strains or species via plasmids (small circular DNA molecules which can replicate independently).
The effects of antibiotic resistance are seen across multiple industries. For example, in medicine, where diseases such as tuberculosis were previously controllable with antibiotics, we are now seeing emergent strains that cannot be killed by historically effective treatments. In farming, the treatment of large herds of livestock with antibiotics is critical to the survival of the animals, and for the production of meat safe for consumption. Use of broad-spectrum antibiotics is wide-ranging in agriculture, but has a similar consequence to the overuse in humans for the development of resistance. There is also the potential for resistant bacteria to move through the food chain via meat or water systems.
Can it be avoided?
The race is on to battle antibiotic resistance. The struggle that drug developers are up against is the speed at which new resistant bacterial strains emerge. Developing and marketing a new drug can take decades and millions of pounds and, at the moment, the bacteria are winning the arms race.
The next part of this blog series will explore the cutting-edge technology being used and research undertaken to combat antibiotic resistance, highlighting the need for international collaboration across multiple industries.
If you would like to find out more on how we help our clients communicate their antimicrobial resistance testing technologies, please get in touch.
By Lizzie Randall, Senior Account Executive at The Scott Partnership.





